bulk bill so common sense tells us it
is also part of the very same service
if you don't bulk bill. Therefore you
would not separate the bandage and
the consultation on your patient claim
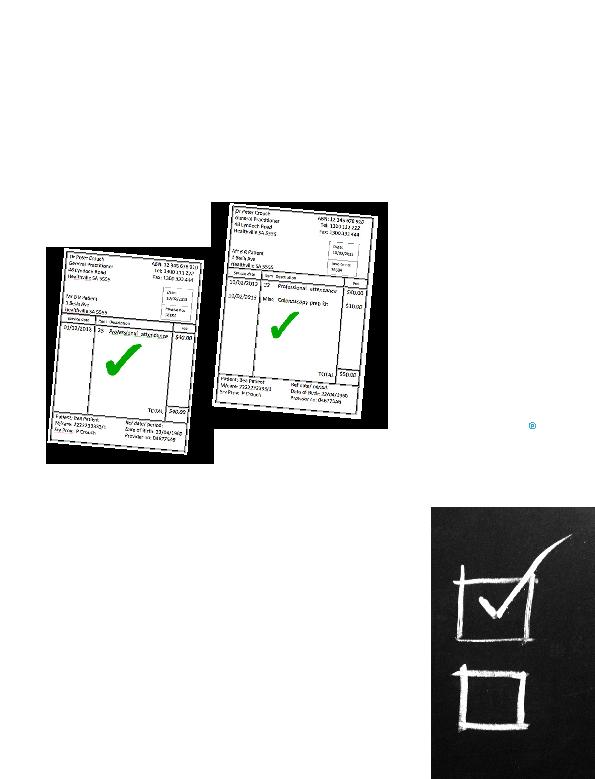
invoice. Instead, it would look like this:
prep kit?
Just to throw a spanner in the
works, what if you have consulted
a patient who presented with a leg
ulcer and your consultation involved
the examination and treatment of
that ulcer (including dressing it), but
then, just as you were finishing up,
the patient said she was having that
colonoscopy you ordered next week
and wondered if you might sell `those
prep kits', which of course you do.
intend to invoice as item 23 for the
ulcer consultation, which was why the
patient came to see you?
to the leg ulcer, so it should not be
added to the total fee for the item 23.
The colonoscopy prep kit should be
itemised separately, as follows:
there really is no need. Everything can
go on the one invoice when you are
doing patient claims and this will still
be fully compliant with the legislation.
clinically relevant services are a
private matter between the doctor and
the patient, and such services should
not be billed to Medicare. As long
as you are not adding inappropriate
extras to the MBS item numbers,
all will be well. Medicare will simply
ignore the items described as `Misc'
(or whatever other description your
practice uses) when they receive the
claim from the patient.
numbers, as it foots much of the bill
patient have agreed upon under your
private contractual arrangement.
Conversely, however, the full amount
you charge for your service must
be included on the invoice and be
disclosed to Medicare that's the
law. So, if you routinely charge your
patients $100 for item 23, this
amount must be fully disclosed to
Medicare on your invoice for that
item number.
mention: Medicare is a fee-for-service
scheme, which means that, subject to
the odd exception, if you provide more
than one service to your patient on the
same day, you can bulk bill one and not
the other. But that's another story.